
 About Ketorol D.T.
About Ketorol D.T.
- KETOROL D.T. from Dr. Reddy’s is the World’s No. 1 Brand for dental pain relief and is trusted by doctors since the past 25+ years.*
- Available in dispersible formulation with fast action within 10 minutes1 of intake.
- Ketorolac is a light-sensitive molecule and KETOROL D.T. comes in Alu-blister packaging to ensure maximum protection from sunlight.
*Data on file
1. Vadivedlu N, et al. Pain Pract. 2015;15(2):175-193. 2. Sadeghein A, et al. J Endod. 1999;25(4):257-259
 Where to Use?
Where to Use?
It is used in the short-term management of moderate postoperative pain.
Dosage and administration
- Ketorolac tablets are recommended for short-term use only (up to 7 days) and are not recommended for chronic use.
- Adults: 20 mg once, followed by 10 mg every 6 hrs, not exceeding 40 mg in a day.
- Elderly: A longer dosing interval, e.g. 6-8 hourly, is advisable in the elderly.
- Children: The safety and efficacy profile of ketorolac in paediatric patients <18 years has not been clinically established.
- For patients receiving parenteral ketorolac, and who are converted to ketorolac oral tablets, the total combined daily dose should not exceed 90 mg and the oral component should not exceed 40 mg on the day the change of formulation is made.
 Safety Advise
Safety Advise
Dosage & administration:
- Adults: 20 mg once followed by 10 mg every 6 hrs.
- Maximum dose: 40 mg
- Maximum Duration: up to 7 days.
- Elderly: longer dosing interval, e.g. 6-8 hourly
Use in specific populations:
The long-term administration of ketorolac tromethamine is not recommended as the incidence of side-effects increases with the duration of treatment.
- Use in Pregnancy and Lactation: Not recommended during pregnancy or lactation.
- Use in Children: Not recommended for use in children under age 16.
- Use in the Elderly: Extra caution and the lowest effective dose should be used.
- Use in Renal, Hepatic & Heart failure patients: Not recommended
 What are the Side Effects?
What are the Side Effects?
- Renal events: Acute renal failure, flank pain with or without haematuria and/or azotaemia, nephritis, hyponatremia, hyperkalaemia, haemolytic uremic syndrome, urinary retention.
- Hypersensitivity reactions: Bronchospasm, laryngeal oedema, asthma, hypotension, flushing, rash, anaphylaxis, and anaphylactoid reactions.
- Gastrointestinal events: Gastrointestinal haemorrhage, peptic ulceration, gastrointestinal perforation, pancreatitis, melena.
- Hematologic events: Postoperative wound hemorrhage, rarely requiring blood transfusion, thrombocytopenia, epistaxis, leukopenia.
- Central nervous system: Convulsions, hallucinations, hyperkinesia, hearing loss, aseptic meningitis, extrapyramidal symptoms.
- Hepatic events: Hepatitis, liver failure, cholestatic jaundice Cardiovascular: pulmonary edema, hypotension, flushing.
- Dermatology: Lyell's syndrome, Stevens-Johnson syndrome, exfoliative dermatitis, maculopapular rash, urticarial.
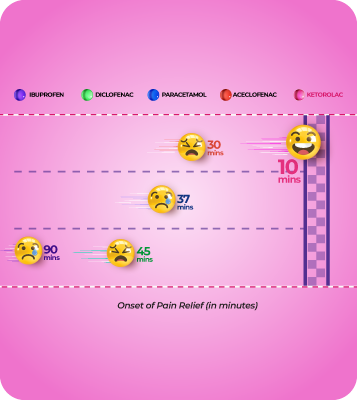 Ketorol Vs. NSAIDs
Ketorol Vs. NSAIDs
- Ketorolac is predominantly prescribed by dental practitioners for monotherapy in dental pain management, followed by diclofenac and aceclofenac.
- Ketorolac is administered across all phases of dental pain and is the most preferred option among the analgesics (monotherapy/combinations) by dental practitioners.
Shukla K, Kiran Pebbili K, Bhagat SV, Rathod R, Kotak BP. Prospective Evaluation of Dental Practitioners'
Knowledge, Attitude, and Practice Toward Adult Dental Pain Management: A Cross-Sectional Multicenter Study. Cureus. 2024 Mar 2;16(3):e55388. doi: 10.7759/cu reus.55388. PMID: 38562370; PMCID: PMC10984245.
Editor's Pick
New treatment techniques in Endodontics
New treatment techniques in Endodontics
New pain management techniques in endodontics, including incision and drainage, re-instrumentation, occlusal reduction, platelet-rich fibrin, and cryotherapy, offer effective relief, improving treatment outcomes.New treatment techniques in Endodontics
ADA guidelines for Temporary Management of Acute Dental Pain
ADA guidelines for Temporary Management of Acute Dental Pain
The ADA recommends short-acting local anesthetics for immediate toothache relief, nonopioid analgesics for post-visit care, and suggests supplemental anesthetics and topical benzocaine for extended management.ADA guidelines for Temporary Management of Acute Dental Pain
Efficacy of Lasers for Postoperative Pain in RCT
Efficacy of Lasers for Postoperative Pain in RCT
Laser therapies like PDT and PBM offer short-term pain relief after root canal treatment, with reduced efficacy over time. They show promise over conventional methods, but further research is needed for long-term use.Efficacy of Lasers for Postoperative Pain in RCT
Laser-Assisted Disinfection in Root Canal Therapy
Laser-Assisted Disinfection in Root Canal Therapy
This study found cryotherapy effectively reduced postoperative pain after root canal treatment, showing results like occlusal reduction but more conservative. Pain decreased in all groups over time, with zero pain reported by day 7.Laser-Assisted Disinfection in Root Canal Therapy
Cryotherapy and Occlusal Reduction for Post-Endodontic Pain
Cryotherapy and Occlusal Reduction for Post-Endodontic Pain
This study found cryotherapy effectively reduced postoperative pain after root canal treatment, showing results like occlusal reduction but more conservative. Pain decreased in all groups over time, with zero pain reported by day 7.Cryotherapy and Occlusal Reduction for Post-Endodontic Pain
American Dental Association (ADA) Guidelines
American Dental Association (ADA) Guidelines
ADA guidelines recommend nonopioid analgesics as first-line therapy for post-extraction pain, with NSAIDs or NSAID-acetaminophen combos preferred. Supplemental anesthetics and minimal opioid use are advised.American Dental Association (ADA) Guidelines
Pop & Go: The Fast Track to Oral Drug Delivery with Dissolving Tablets
Pop & Go: The Fast Track to Oral Drug Delivery with Dissolving Tablets
Pop & Go: The Fast Track to Oral Drug Delivery with Dissolving TabletsPop & Go: The Fast Track to Oral Drug Delivery with Dissolving Tablets
Clinical Guidance for Optimal Endodontic Management of Traumatized Permanent Teeth
Clinical Guidance for Optimal Endodontic Management of Traumatized Permanent Teeth
Clinical Guidance for Optimal Endodontic Management of Traumatized Permanent TeethClinical Guidance for Optimal Endodontic Management of Traumatized Permanent Teeth
Odontalgia Odyssey Navigating Dental Pain Management in India
Odontalgia Odyssey Navigating Dental Pain Management in India
Odontalgia Odyssey Navigating Dental Pain Management in IndiaOdontalgia Odyssey Navigating Dental Pain Management in India
Challenges and Insights: Understanding the Raise of Dental Caries in India
Challenges and Insights: Understanding the Raise of Dental Caries in India
Challenges and Insights: Understanding the Raise of Dental Caries in IndiaChallenges and Insights: Understanding the Raise of Dental Caries in India
Videos Speakers
Pain after root canal treatment with various apical finishing sizes
Pain after root canal treatment with various apical finishing sizes
A recent study revealed that the size of apical preparation had a significant impact on postoperative pain levels. The results of this study were published in the journal BMC Oral Health.
In this study, fifty teeth belonging to twenty-five individuals were separated into two equal groups, with twenty-five teeth in each group using E3 Azure rotary files. Group A was expanded by two sizes in relation to the Initial Binding File (IBF), extending to 40#/0.04 for the distal canals and 35#/0.04 for the mesial canals. Group B, on the other hand, was expanded by three sizes larger than the IBF: 45#/0.04 for the distal canals and 40#/0.04 for mesial canals. Patients were asked to rate their pain levels on a modified VAS form and describe their pain intensity at twelve, twenty-four, and seventy-two hours, as well as after a week. VAS data were analyzed using Freidman's test, Nemenyi post hoc test for intragroup comparisons and signed-rank test for intergroup comparisons.
The outcomes revealed that irrespective of the timing of the measurement, an enlargement of the apical preparation was significantly linked to increased pain scores (p value < 0.001). In both groups, there was a significant decline in reported pain scores over time, with scores at twelve-and twenty-four hours post-treatment significantly higher than those at other intervals (p value < 0.001). Additionally, pain scores at three days post-treatment were significantly higher than those at one week (p value < 0.001).
Thus, it can be concluded that apical preparation size significantly influenced postoperative pain levels.
Pain after root canal treatment with various apical finishing sizes
Pain after root canal treatment with various apical finishing sizes
A recent study revealed that the size of apical preparation had a significant impact on postoperative pain levels. The results of this study were published in the journal BMC Oral Health.
In this study, fifty teeth belonging to twenty-five individuals were separated into two equal groups, with twenty-five teeth in each group using E3 Azure rotary files. Group A was expanded by two sizes in relation to the Initial Binding File (IBF), extending to 40#/0.04 for the distal canals and 35#/0.04 for the mesial canals. Group B, on the other hand, was expanded by three sizes larger than the IBF: 45#/0.04 for the distal canals and 40#/0.04 for mesial canals. Patients were asked to rate their pain levels on a modified VAS form and describe their pain intensity at twelve, twenty-four, and seventy-two hours, as well as after a week. VAS data were analyzed using Freidman's test, Nemenyi post hoc test for intragroup comparisons and signed-rank test for intergroup comparisons.
The outcomes revealed that irrespective of the timing of the measurement, an enlargement of the apical preparation was significantly linked to increased pain scores (p value < 0.001). In both groups, there was a significant decline in reported pain scores over time, with scores at twelve-and twenty-four hours post-treatment significantly higher than those at other intervals (p value < 0.001). Additionally, pain scores at three days post-treatment were significantly higher than those at one week (p value < 0.001).
Thus, it can be concluded that apical preparation size significantly influenced postoperative pain levels.
Assessment of postoperative pain following the use of dexamethasone intracanal rinse for irreversible pulpitis
Assessment of postoperative pain following the use of dexamethasone intracanal rinse for irreversible pulpitis
A recent study has shown that dexamethasone is superior to saline in relieving postoperative pain when utilized as the final intracanal rinse after root canal instrumentation. This study's findings were published in the Journal of the College of Physicians and Surgeons Pakistan.
Sixty patients aged 18 to 50 years, who had been diagnosed with symptomatic irreversible pulpitis were specifically chosen based on set criteria. Root canal therapy (RCT) was initiated under rubber dam after obtaining informed consent. The treatment included a pulpectomy followed by canal preparation. Patients were divided into two groups: Group A (the experimental group) received dexamethasone (4 mg/mL in a 5-mL syringe) as a final rinse, and Group B (the control group) received saline as the final rinse. They were followed up after 1 week to determine the improvement of their pain. Following data collection, teeth were filled, and permanent restoration was placed. The Chi-square test was utilized for the analysis of the data.
Dexamethasone showed a significantly higher efficacy compared to saline as a final intracanal rinse, 86.67% and 20.0%, respectively (p value < 0.05), in alleviating postoperative pain in teeth diagnosed with symptomatic irreversible pulpitis.
The above study demonstrated that dexamethasone has greater efficacy compared to saline in alleviating postoperative pain when utilized as the final intracanal rinse following root canal instrumentation.
Assessment of postoperative pain following the use of dexamethasone intracanal rinse for irreversible pulpitis
Assessment of postoperative pain following the use of dexamethasone intracanal rinse for irreversible pulpitis
A recent study has shown that dexamethasone is superior to saline in relieving postoperative pain when utilized as the final intracanal rinse after root canal instrumentation. This study's findings were published in the Journal of the College of Physicians and Surgeons Pakistan.
Sixty patients aged 18 to 50 years, who had been diagnosed with symptomatic irreversible pulpitis were specifically chosen based on set criteria. Root canal therapy (RCT) was initiated under rubber dam after obtaining informed consent. The treatment included a pulpectomy followed by canal preparation. Patients were divided into two groups: Group A (the experimental group) received dexamethasone (4 mg/mL in a 5-mL syringe) as a final rinse, and Group B (the control group) received saline as the final rinse. They were followed up after 1 week to determine the improvement of their pain. Following data collection, teeth were filled, and permanent restoration was placed. The Chi-square test was utilized for the analysis of the data.
Dexamethasone showed a significantly higher efficacy compared to saline as a final intracanal rinse, 86.67% and 20.0%, respectively (p value < 0.05), in alleviating postoperative pain in teeth diagnosed with symptomatic irreversible pulpitis.
The above study demonstrated that dexamethasone has greater efficacy compared to saline in alleviating postoperative pain when utilized as the final intracanal rinse following root canal instrumentation.
Cannabidiol Found Effective as an Analgesic for Acute Dental Pain
Cannabidiol Found Effective as an Analgesic for Acute Dental Pain
This study evaluated the efficacy and safety of cannabidiol (CBD) as an analgesic for acute dental pain, a condition for which nonopioid treatments are limited. In a randomized, placebo-controlled clinical trial, 61 patients with moderate to severe toothache were assigned to one of three groups: CBD10 (10 mg/kg), CBD20 (20 mg/kg), or placebo. Participants received a single oral dose, and pain was assessed over 3 hours.
The primary outcome was pain reduction using a visual analog scale (VAS), while secondary outcomes included pain intensity, time to significant relief, maximum pain relief, bite force changes, psychoactive effects, mood alterations, and other adverse events.
Both CBD groups showed significant reductions in VAS pain scores compared to baseline and placebo, with a maximum median reduction of 73% at 180 minutes (P < 0.05). CBD20 demonstrated a faster onset of pain relief than CBD10 (15 vs. 30 minutes), with both groups achieving maximum relief at 180 minutes. The number needed to treat was 3.1 for CBD10 and 2.4 for CBD20. Bite force significantly increased in both CBD groups (P < 0.05) but not in the placebo group, with CBD20 showing significant changes compared to placebo at 90 and 180 minutes.
Adverse effects, including sedation, diarrhea, and abdominal pain, were more common in CBD groups (P < 0.05). This trial provides initial evidence that oral CBD is an effective and safe alternative analgesic for acute dental pain.
Cannabidiol Found Effective as an Analgesic for Acute Dental Pain
Cannabidiol Found Effective as an Analgesic for Acute Dental Pain
This study evaluated the efficacy and safety of cannabidiol (CBD) as an analgesic for acute dental pain, a condition for which nonopioid treatments are limited. In a randomized, placebo-controlled clinical trial, 61 patients with moderate to severe toothache were assigned to one of three groups: CBD10 (10 mg/kg), CBD20 (20 mg/kg), or placebo. Participants received a single oral dose, and pain was assessed over 3 hours.
The primary outcome was pain reduction using a visual analog scale (VAS), while secondary outcomes included pain intensity, time to significant relief, maximum pain relief, bite force changes, psychoactive effects, mood alterations, and other adverse events.
Both CBD groups showed significant reductions in VAS pain scores compared to baseline and placebo, with a maximum median reduction of 73% at 180 minutes (P < 0.05). CBD20 demonstrated a faster onset of pain relief than CBD10 (15 vs. 30 minutes), with both groups achieving maximum relief at 180 minutes. The number needed to treat was 3.1 for CBD10 and 2.4 for CBD20. Bite force significantly increased in both CBD groups (P < 0.05) but not in the placebo group, with CBD20 showing significant changes compared to placebo at 90 and 180 minutes.
Adverse effects, including sedation, diarrhea, and abdominal pain, were more common in CBD groups (P < 0.05). This trial provides initial evidence that oral CBD is an effective and safe alternative analgesic for acute dental pain.
The effect of various desensitizers on pulpal blood flow after full crown preparation using laser Doppler flowmetry
The effect of various desensitizers on pulpal blood flow after full crown preparation using laser Doppler flowmetry
In a recent study, similar levels of effectiveness were observed in treating dentine hypersensitivity and pulpal blood flow with Bifluoride 12, Teethmate, and Copal Varnish. This study’s findings were published in the journal Odontology.
18 patients with a total of 42 teeth suffering from dentine hypersensitivity after full crown preparations were randomly divided to receive treatment with Bifluoride 12, Teethmate, or Copal Varnish. The severity of dentine hypersensitivity was assessed using a Schiff air index (SAI) and visual analog scale (VAS). The assessment of pulpal blood flow involved the use of laser Doppler flowmetry (LDF), with the findings recorded in perfusion units (PU). Evaluations were conducted at the initial stage, after five minutes, after seven days, and after one month subsequent to the administration of desensitizing agents. Statistical analysis was carried out using Wilcoxon and two-way ANOVA tests (p value < 0.05).
The tested desensitizers did not show any significant difference in terms of VAS and PU values. VAS values significantly decreased at seven days and one month after the desensitizers were applied, compared to the baseline in all groups. Only the Copal Varnish group exhibited a notable difference in PU values at the five-minute and seven-day intervals post-desensitizer application (p value < 0.05). A statistically significant difference was found between different time points in relation to SAI scores in all groups (p value < 0.05).
Thus, it can be concluded that Bifluoride 12, Teethmate, and Copal Varnish demonstrated similar effectiveness in managing dentine hypersensitivity and pulpal blood flow. To fully evaluate their impact on pulpal status, it is important to conduct long-term clinical trials with larger sample sizes and histological studies.
The effect of various desensitizers on pulpal blood flow after full crown preparation using laser Doppler flowmetry
The effect of various desensitizers on pulpal blood flow after full crown preparation using laser Doppler flowmetry
In a recent study, similar levels of effectiveness were observed in treating dentine hypersensitivity and pulpal blood flow with Bifluoride 12, Teethmate, and Copal Varnish. This study’s findings were published in the journal Odontology.
18 patients with a total of 42 teeth suffering from dentine hypersensitivity after full crown preparations were randomly divided to receive treatment with Bifluoride 12, Teethmate, or Copal Varnish. The severity of dentine hypersensitivity was assessed using a Schiff air index (SAI) and visual analog scale (VAS). The assessment of pulpal blood flow involved the use of laser Doppler flowmetry (LDF), with the findings recorded in perfusion units (PU). Evaluations were conducted at the initial stage, after five minutes, after seven days, and after one month subsequent to the administration of desensitizing agents. Statistical analysis was carried out using Wilcoxon and two-way ANOVA tests (p value < 0.05).
The tested desensitizers did not show any significant difference in terms of VAS and PU values. VAS values significantly decreased at seven days and one month after the desensitizers were applied, compared to the baseline in all groups. Only the Copal Varnish group exhibited a notable difference in PU values at the five-minute and seven-day intervals post-desensitizer application (p value < 0.05). A statistically significant difference was found between different time points in relation to SAI scores in all groups (p value < 0.05).
Thus, it can be concluded that Bifluoride 12, Teethmate, and Copal Varnish demonstrated similar effectiveness in managing dentine hypersensitivity and pulpal blood flow. To fully evaluate their impact on pulpal status, it is important to conduct long-term clinical trials with larger sample sizes and histological studies.
Comparison of tramadol-celecoxib co-crystal with tramadol or placebo for managing acute moderate-to-severe pain following oral surgery
Comparison of tramadol-celecoxib co-crystal with tramadol or placebo for managing acute moderate-to-severe pain following oral surgery
According to a recent study, the co-crystal of tramadol-celecoxib (CTC) showed superior pain relief when compared to tramadol or placebo and also displayed an improved benefit/risk profile in comparison to tramadol. The findings were published in the journal Advances in Therapy.
A total of 726 adults were randomly assigned to five groups (2:2:2:2:1). Different treatment groups were assigned varying doses of medication, such as twice daily 100mg CTC (n = 164), 150 mg CTC (n = 160), or 200 mg CTC (n = 160), four times a day 100mg tramadol (n = 159), or four times a day placebo (n = 83). Twice daily placebo was also given to individuals in the CTC groups. Total of pain intensity differences measured from 0 to 4 hours (SPID0–4; visual analog scale) was the primary endpoint. The key secondary endpoints of the study assessed rescue medication use and 4-hour 50% responder rates. Safety endpoints included laboratory measures, adverse events, and the Opioid-Related Symptom Distress Scale (OR-SDS) score.
All CTC doses were more effective than placebo (P value < 0.001) for primary and key secondary endpoints. Additionally, they exhibited superiority over tramadol for SPID0-4 (Analysis of covariance least squares mean differences [95% CI]: - 37.1 [- 56.5, - 17.6], - 40.2 [- 59.7, - 20.6], and - 41.7 [- 61.2, - 22.2] for 100 mg , 150 mg , and 200 mg CTC, respectively; P value < 0.001) and 4-hour 50% responder rate. The 4-hour 50% responder rates were 32.9% for CTC 100 mg, 33.8% for CTC 150 mg, 40.6% for CTC 200 mg, 20.1% for tramadol, and 7.2% for placebo groups, respectively. Rescue medication consumption was less in the 100-mg (P value = 0.013) and 200-mg (P value = 0.003) CTC groups in comparison to the tramadol group. Tramadol by itself exhibited the highest occurrence of adverse events and OR-SDS scores.
Thus, it can be concluded that CTC provided superior pain relief compared to tramadol or placebo and also showed an improved benefit/risk profile in comparison to tramadol.
Comparison of tramadol-celecoxib co-crystal with tramadol or placebo for managing acute moderate-to-severe pain following oral surgery
Comparison of tramadol-celecoxib co-crystal with tramadol or placebo for managing acute moderate-to-severe pain following oral surgery
According to a recent study, the co-crystal of tramadol-celecoxib (CTC) showed superior pain relief when compared to tramadol or placebo and also displayed an improved benefit/risk profile in comparison to tramadol. The findings were published in the journal Advances in Therapy.
A total of 726 adults were randomly assigned to five groups (2:2:2:2:1). Different treatment groups were assigned varying doses of medication, such as twice daily 100mg CTC (n = 164), 150 mg CTC (n = 160), or 200 mg CTC (n = 160), four times a day 100mg tramadol (n = 159), or four times a day placebo (n = 83). Twice daily placebo was also given to individuals in the CTC groups. Total of pain intensity differences measured from 0 to 4 hours (SPID0–4; visual analog scale) was the primary endpoint. The key secondary endpoints of the study assessed rescue medication use and 4-hour 50% responder rates. Safety endpoints included laboratory measures, adverse events, and the Opioid-Related Symptom Distress Scale (OR-SDS) score.
All CTC doses were more effective than placebo (P value < 0.001) for primary and key secondary endpoints. Additionally, they exhibited superiority over tramadol for SPID0-4 (Analysis of covariance least squares mean differences [95% CI]: - 37.1 [- 56.5, - 17.6], - 40.2 [- 59.7, - 20.6], and - 41.7 [- 61.2, - 22.2] for 100 mg , 150 mg , and 200 mg CTC, respectively; P value < 0.001) and 4-hour 50% responder rate. The 4-hour 50% responder rates were 32.9% for CTC 100 mg, 33.8% for CTC 150 mg, 40.6% for CTC 200 mg, 20.1% for tramadol, and 7.2% for placebo groups, respectively. Rescue medication consumption was less in the 100-mg (P value = 0.013) and 200-mg (P value = 0.003) CTC groups in comparison to the tramadol group. Tramadol by itself exhibited the highest occurrence of adverse events and OR-SDS scores.
Thus, it can be concluded that CTC provided superior pain relief compared to tramadol or placebo and also showed an improved benefit/risk profile in comparison to tramadol.
How would you rate this Medshorts
Thank you !
Your rating has been recorded.
Videos Speakers
Ketorol-DT 1
Ketorol-DT 1, Dental, Dental & Oral Health, Dentist, Docvidya, Brands, Dental Pain, Ketorolac, Ketorolac Tromethamine, Acute Dental Pain, NSAID
Below fields are needed for webinar purpose.





























