 Why Vono
Why Vono
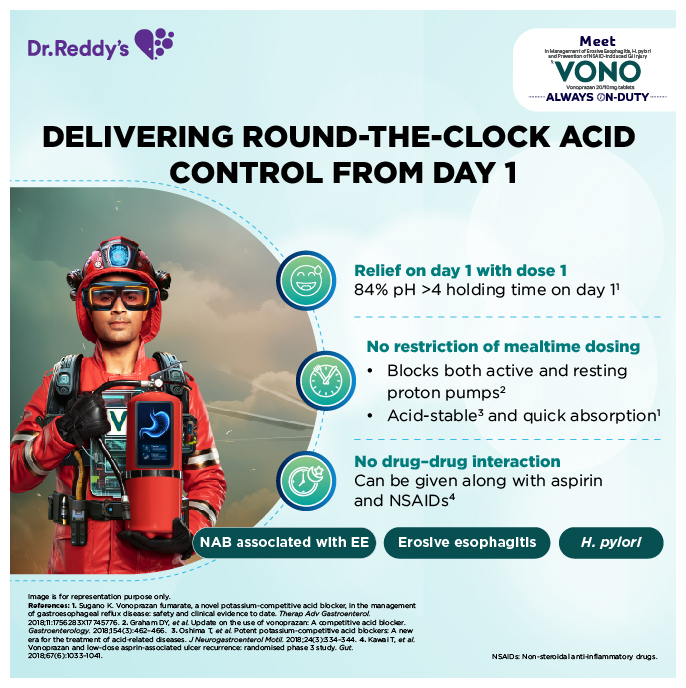
Vonoprazan, a novel class of Potassium Competitive Acid Blocker has been introduced in the space of Anti-peptic ulcerants post 3 long decades of PPI existence as the best alternative. This superior molecule promises to be the future with its key attributes of 24-hour pH > 4 holding time ratio, peak action with its first dose, and immediate symptomatic relief & no restriction of mealtime dosing for best patient outcomes. Dr. Reddys who has been at the forefront in Gastroenterology therapy are among the first few top Indian Pharma Companies to launch the patented molecule Vono ( Vonoprazan) along with a non-exclusive patent licensing agreement with manufacturers to commercialize Vono (Vonoprazan) in India.
 Where to Use
Where to Use
•Treatment of reflux esophagitis (RE)
•Treatment of gastric ulcer (GU)
•Treatment of duodenal ulcer (DU)
•Prevention of reoccurrence of gastric ulcer or duodenal ulcer during low-dose aspirin administration
•Prevention of reoccurrence of gastric ulcer or duodenal ulcer during NSAIDs administration.
•Adjunct to Helicobacter pylori (H. pylori) eradication associated with: Gastric ulcer, duodenal ulcer, gastric MALT lymphoma, idiopathic thrombocytopenic purpura, the stomach after endoscopic resection of early stage cancer or Helicobacter Pylori gastritis.
How to Use
•Reflux esophagitis (erosive esophagitis)
The usual dose is 20 mg of vonoprazan once a day. Administration should be limited to 4 weeks. However, when the effect is insufficient, treatment may be continued for up to 8 weeks.
•Gastric ulcer: The usual dose is 20 mg of vonoprazan once a day. Administration should be limited to 8 weeks.
•Duodenal ulcer: The usual dose is 20 mg of vonoprazan once a day. Administration should be limited to 6 weeks.
•Prevention of recurrence of gastric ulcer or duodenal ulcer during low-dose aspirin administration. The usual dose is 10 mg of vonoprazan once a day.
•Adjunct to Helicobacter pylori eradication: Usually, the following 3 drugs are orally administered at the same time twice daily for 7 days: 20 mg vonoprazan, 750 mg amoxicillin hydrate, and 200 mg clarithromycin. The dose of clarithromycin may be appropriately increased as required; however, the upper limit is 400 mg twice daily or physician judgement.
When Helicobacter pylori eradication treatment with 3 drugs consisting of a proton pump inhibitor, amoxicillin hydrate, and clarithromycin fails, alternative treatment with the following 3 drugs is recommended; 20 mg vonoprazan, 750 mg amoxicillin hydrate, and 250 mg metronidazole, orally administered at the same time twice daily for 7 days. The doses of antibiotic should follow the respective label recommendations for H. pylori eradication.
Special Patient Populations
Elderly Patients:
Since the physiological functions such as hepatic or renal function are decreased in elderly patients in general, vonoprazan should be carefully administered.
Paediatric Patients:
Vonoprazan has not been studied in patients under 18 years of age.
Impaired Renal Function:
a.Healing of Erosive Esophagitis:
The recommended dosage of Vonoprazan in adult patients with renal impairment is described in Table 1 below.
Safety Advice
Use in Special Populations (Such as Pregnant Women, Lactating Women, Paediatric Patients, Geriatric Patients, etc.)
Pregnancy
No clinical studies have been conducted to date to evaluate vonoprazan in subjects who are pregnant. In a rat toxicology study, embryo-foetal toxicity was observed following exposure of more than approximately 28 times of the exposure (AUC) at the maximum clinical dose (40 mg/day) of vonoprazan. As a precaution, vonoprazan should not be administered to women who are or may be pregnant, unless the expected therapeutic benefit is thought to outweigh any possible risk.
Lactation
No clinical studies have been conducted to date to evaluate vonoprazan in subjects who are lactating are lactating. It is unknown whether vonoprazan is excreted in human milk. In animal studies it has been shown that vonoprazan was excreted in milk. During treatment with vonoprazan, nursing should be avoided if the administration of this drug is necessary for the mother.
Pediatric use
The safety and effectiveness of vonoprazan is not established in pediatric patients.
Geriatric use
No overall differences in safety or effectiveness were observed between these patients and younger adult patients, and other reported clinical experience has not identified differences in responses between the geriatric and younger adult patients, but greater sensitivity of some older individuals cannot be ruled out.
No clinically meaningful differences in the pharmacokinetics of vonoprazan are predicted in patients 65 years of age and older compared to younger adult patients.
Renal Impairment
Healing of Erosive Esophagitis: No dosage adjustment of vonoprazan is recommended in patients with mild to moderate renal impairment (eGFR 30 to 89 mL/min). Dosage reduction is recommended in patients with severe renal impairment (eGFR < 30 mL/min). Maintenance of Healed Erosive Esophagitis: No dosage adjustment of vonoprazan is recommended in patients with any degree of renal impairment. Treatment of H. pylori Infection: Use of vonoprazan is not recommended for the treatment of H. pylori infection in patients with severe renal impairment (eGFR < 30 mL/min).
Hepatic Impairment
Healing of Erosive Esophagitis: No dosage adjustment of vonoprazan is recommended in patients with mild hepatic impairment (Child-Pugh A). Dosage reduction is recommended in patients with moderate to severe hepatic impairment (Child-Pugh Class B and C). Maintenance of Healed Erosive Esophagitis: No dosage adjustment of vonoprazan for the maintenance of healed erosive esophagitis is recommended in patients with any degree of hepatic impairment. Treatment of H. pylori Infection: Use of vonoprazan is not recommended in patients with moderate to severe hepatic impairment (Child-Pugh Class B and C).
Effects on ability to drive and use machines
The influence of vonoprazan on the ability to drive or use machines is unknown.
Side Effects
Contraindications
•Vonoprazan is contraindicated in patients with a known hypersensitivity to vonoprazan or any component of Vonoprazan. Reactions have included anaphylactic shock.
•Vonoprazan is contraindicated with rilpivirine-containing products.
•For information about contraindications of antibacterial agents (clarithromycin and amoxicillin) indicated in combination with Vonoprazan, refer to the Contraindications section of the corresponding prescribing information.
Special Warnings and Precautions for Use
Presence of Gastric Malignancy
In adults, symptomatic response to therapy with Vonoprazan does not preclude the presence of gastric malignancy. Consider additional follow-up and diagnostic testing in patients who have a suboptimal response or an early symptomatic relapse after completing treatment with Vonoprazan. In older patients, also consider endoscopy.
Acute Tubulointerstitial Nephritis
Aute tubulointerstitial nephritis (TIN) has been reported with Vonoprazan. If suspected, discontinue Vonoprazan and evaluate patients with suspected acute TIN.
Clostridioides difficile-Associated Diarrhoea
Published observational studies suggest that proton pump inhibitors (PPIs) may be associated with an increased risk of Clostridioides difficile-associated diarrhea (CDAD), especially in hospitalized patients. Vonoprazan, another drug that blocks the proton pump to inhibit gastric acid production, may also increase the risk of CDAD. Consider CDAD in patients with diarrhoea that does not improve. Use the shortest duration of Vonoprazan appropriate to the condition being treated.
CDAD has been reported with use of nearly all antibacterial agents. For more information specific to antibacterial agents (clarithromycin and amoxicillin) indicated for use in combination with Vonoprazan, refer to Warnings and Precautions section of the corresponding prescribing information.
Bone Fracture
Several published observational studies suggest that PPI therapy may be associated with an increased risk for osteoporosis-related fractures of the hip, wrist or spine. The risk of fracture was increased in patients who received high-dose, defined as multiple daily doses, and long-term therapy (a year or longer). Bone fracture, including osteoporosis-related fracture, has also been reported with vonoprazan. Use the shortest duration of Vonoprazan appropriate to the condition being treated. Patients at risk for osteoporosis-related fractures should be managed according to the established treatment guidelines.
Severe Cutaneous Adverse Reactions
Severe cutaneous adverse reactions, including Stevens-Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN) have been reported with Vonoprazan. Discontinue Vonoprazan at the first signs or symptoms of severe cutaneous adverse reactions or other signs of hypersensitivity and consider further evaluation.
Vitamin B12 (Cobalamin) Deficiency
Long-term use of acid-suppressing drugs can lead to malabsorption of Vitamin B12 caused by hypo- or achlorhydria. Vitamin B12 deficiency has been reported postmarketing with vonoprazan. If clinical symptoms consistent with Vitamin B12 deficiency are observed in patients treated with Vonoprazan consider further workup.
Hypomagnesemia and Mineral Metabolism
Hypomagnesemia has been reported postmarketing with vonoprazan. Hypomagnesemia may lead to hypocalcemia and/or hypokalemia and may exacerbate underlying hypocalcemia in at-risk patients.
Consider monitoring magnesium levels prior to initiation of Vonoprazan and periodically in patients expected to be on prolonged treatment, in patients taking drugs that may have increased toxicity in the presence of hypomagnesemia (e.g., digoxin), or drugs that may cause hypomagnesemia (e.g., diuretics). Treatment of hypomagnesemia may require magnesium replacement and discontinuation of Vonoprazan.
Consider monitoring magnesium and calcium levels prior to initiation of Vonoprazan and periodically while on treatment in patients with a preexisting risk of hypocalcemia (e.g., hypoparathyroidism). Supplement with magnesium and/or calcium, as necessary. If hypocalcemia is refractory to treatment, consider discontinuing Vonoprazan.
Interactions with Diagnostic Investigations for Neuroendocrine Tumors
Serum chromogranin A (CgA) levels increase secondary to drug-induced decreases in gastric acidity. The increased CgA level may cause false positive results in diagnostic investigations for neuroendocrine tumors. Temporarily discontinue Vonoprazan treatment at least 14 days before assessing CgA levels and consider repeating the test if initial CgA levels are high. If serial tests are performed (e.g., for monitoring), the same commercial laboratory should be used for testing, as reference ranges between tests may vary.
Fundic Gland Polyps
Use of Vonoprazan is associated with a risk of fundic gland polyps that increases with long-term use, especially beyond one year. Fundic gland polyps have been reported with vonoprazan in clinical trials and post-marketing use with PPIs. Most patients who developed fundic gland polyps were asymptomatic and fundic gland polyps were identified incidentally on endoscopy. Use the shortest duration of Vonoprazan appropriate to the condition being treated.
Drug Interactions:
Table 5 and Table 6 include drugs with clinically important drug interactions and interaction with diagnostics when administered concomitantly with Vonoprazan and instructions for preventing or managing them.
These recommendations are based on either drug interaction trials or predicted interactions due to the expected magnitude of interaction and potential for serious adverse reactions or loss of efficacy.
Consult the labeling of concomitantly used drugs to obtain further information about interactions with Vonoprazan.
Decoding The Clinical Effectiveness of Vonoprazan in Helicobacter pylori Eradication!
Recognizing The Clinical Potency of Vonoprazan in Diverse Gastric Acid Complications!
Recognizing The Clinical Potency of Vonoprazan in Diverse Gastric Acid Complications!
Vonoprazan: The Smarter Solution for GERD and H. pylori Eradication!Recognizing The Clinical Potency of Vonoprazan in Diverse Gastric Acid Complications!
Have You Figured Out the Wide-Spectrum Clinical Advantages of Vonoprazan for Gastric Acid Complications?
Have You Figured Out the Wide-Spectrum Clinical Advantages of Vonoprazan for Gastric Acid Complications?
Unlock Gastric Relief Secrets with Vonoprazan...Have You Figured Out the Wide-Spectrum Clinical Advantages of Vonoprazan for Gastric Acid Complications?
Are You Abreast About Diverse Gastric Ulcer Types and the Clinical Benefits of Vonoprazan Against Them?
Are You Abreast About Diverse Gastric Ulcer Types and the Clinical Benefits of Vonoprazan Against Them?
Breakthrough Ulcer Therapy Inside...Are You Abreast About Diverse Gastric Ulcer Types and the Clinical Benefits of Vonoprazan Against Them?
Endoscopic Management Strategies for GERD: Are They Worthy of Attention?
Endoscopic Management Strategies for GERD: Are They Worthy of Attention?
Explore TIF 2.0 as a less invasive solution for managing GERD.Endoscopic Management Strategies for GERD: Are They Worthy of Attention?
Cognizant of the Fact That Refractory Gastroesophageal Reflux Disease Can be Detected by Quantification of Bacterial Overgrowth in Small Intestine?
Cognizant of the Fact That Refractory Gastroesophageal Reflux Disease Can be Detected by Quantification of Bacterial Overgrowth in Small Intestine?
Explore how bacterial overgrowth may uncover refractory GERD issues.Cognizant of the Fact That Refractory Gastroesophageal Reflux Disease Can be Detected by Quantification of Bacterial Overgrowth in Small Intestine?
Apprised of the Hemostatic Strategies and Their Intricacies for Management of Upper Gastrointestinal Bleeding?
Apprised of the Hemostatic Strategies and Their Intricacies for Management of Upper Gastrointestinal Bleeding?
Don't Miss: Endoscopy's Role In GI BleedingApprised of the Hemostatic Strategies and Their Intricacies for Management of Upper Gastrointestinal Bleeding?
Preference for Diagnostic Testing with pH and Impedance Monitoring Over Empiric PPI Trial: Are There Any Benefits?
Preference for Diagnostic Testing with pH and Impedance Monitoring Over Empiric PPI Trial: Are There Any Benefits?
Discover why pH and impedance monitoring may be better than empiric PPI trials for reflux diagnosis.Preference for Diagnostic Testing with pH and Impedance Monitoring Over Empiric PPI Trial: Are There Any Benefits?
CYP2C19 Polymorphism: PPI vs. VONOprazan
CYP2C19 Polymorphism: PPI vs. VONOprazan
CYP2C19 Polymorphism: PPI Efficacy vs. VonoprazanRecognizing The Novel Diagnostic Tools for H. pylori Infection
Recognizing The Novel Diagnostic Tools for H. pylori Infection
Accurate Diagnosis of H. pylori: Novel Tools You Should Know AboutRecognizing The Novel Diagnostic Tools for H. pylori Infection
Safety and efficacy of dapagliflozin in individuals diagnosed with acute heart failure
Safety and efficacy of dapagliflozin in individuals diagnosed with acute heart failure
A recent study demonstrated that the early administration of dapagliflozin during the acute heart failure (AHF) hospitalization is safe and serves as a component of guideline-directed medical therapy (GDMT) optimization. Additionally, dapagliflozin may be associated with improved diuresis in patients with AHF. This study's findings were published in the Journal of the American College of Cardiology.
A total of 240 patients were enrolled in this multicenter trial, where they were randomized to receive either dapagliflozin 10 mg once daily or structured usual care with protocolized diuretic titration within a period of 24 hours of hospital admission for hypervolemic AHF. The primary outcome of the study, diuretic efficiency, was assessed by comparing the cumulative weight change per cumulative loop diuretic dose between the two treatment groups.
Administration of dapagliflozin resulted in a reduction in loop diuretic doses (560 mg [Q1-Q3: 260-1,150 mg] compared to 800 mg [Q1-Q3: 380-1,715 mg]) and a reduced need for intravenous diuretic adjustments to achieve comparable weight loss as standard treatment. Commencing dapagliflozin early did not elevate the occurrence of safety issues related to diabetes, kidney function, or cardiovascular health. Additionally, dapagliflozin was linked to an enhancement in median 24-hour natriuresis and urine output, facilitating quicker hospital discharge throughout the study duration.
Thus, it can be concluded that the early use of dapagliflozin during AHF hospitalization is considered safe and fulfills a component of optimizing GDMT. Additionally, dapagliflozin may lead to improved diuresis in individuals with AHF.
Safety and efficacy of dapagliflozin in individuals diagnosed with acute heart failure
Safety and efficacy of dapagliflozin in individuals diagnosed with acute heart failure
A recent study demonstrated that the early administration of dapagliflozin during the acute heart failure (AHF) hospitalization is safe and serves as a component of guideline-directed medical therapy (GDMT) optimization. Additionally, dapagliflozin may be associated with improved diuresis in patients with AHF. This study's findings were published in the Journal of the American College of Cardiology.
A total of 240 patients were enrolled in this multicenter trial, where they were randomized to receive either dapagliflozin 10 mg once daily or structured usual care with protocolized diuretic titration within a period of 24 hours of hospital admission for hypervolemic AHF. The primary outcome of the study, diuretic efficiency, was assessed by comparing the cumulative weight change per cumulative loop diuretic dose between the two treatment groups.
Administration of dapagliflozin resulted in a reduction in loop diuretic doses (560 mg [Q1-Q3: 260-1,150 mg] compared to 800 mg [Q1-Q3: 380-1,715 mg]) and a reduced need for intravenous diuretic adjustments to achieve comparable weight loss as standard treatment. Commencing dapagliflozin early did not elevate the occurrence of safety issues related to diabetes, kidney function, or cardiovascular health. Additionally, dapagliflozin was linked to an enhancement in median 24-hour natriuresis and urine output, facilitating quicker hospital discharge throughout the study duration.
Thus, it can be concluded that the early use of dapagliflozin during AHF hospitalization is considered safe and fulfills a component of optimizing GDMT. Additionally, dapagliflozin may lead to improved diuresis in individuals with AHF.
Effect of ferric derisomaltose on cardiovascular and non-cardiovascular events in patients with iron deficiency anemia and heart failure
Effect of ferric derisomaltose on cardiovascular and non-cardiovascular events in patients with iron deficiency anemia and heart failure
A recent study found that the administration of intravenous ferric derisomaltose (FDI) in patients diagnosed with both iron deficiency anemia and heart failure with reduced left ventricular ejection fraction has been found to improve their quality of life and may decrease cardiovascular events. This study’s results were published in the Journal of Cardiac Failure.
In the IRONMAN trial, patients with heart failure, iron deficiency (ferritin <100 µg/L or transferrin saturation of <20%), and a left ventricular ejection fraction of ≤45% were enrolled. Out of the total, 68% (n= 771) had anemia (hemoglobin less than 12 g/dL for women and less than 13 g/dL for men). Patients were then randomly assigned to either FDI (n = 397) or usual care (n = 374) and were followed for a median duration of 2.6 years. The primary endpoint of the study was recurrent hospitalization for heart failure and cardiovascular death.
The occurrence of recurrent hospitalization for heart failure and cardiovascular death was less frequent among individuals assigned to FDI (rate ratio 0.78, 95% confidence interval of 0.61-1.01, and the p-value = 0.063). Similarly, the first event analysis for cardiovascular hospitalization or death for heart failure showed similar results (hazard ratio of 0.77, 95% confidence interval of 0.62-0.96 ; p-value = 0.022). Additionally, patients who were randomized to FDI reported better quality of life scores for overall (p-value = 0.013) and physical domain (p-value = 0.00093) at 4 months, as measured by the Minnesota Living with Heart Failure questionnaire.
The above study demonstrated that the administration of intravenous FDI improves the quality of life in patients diagnosed with both iron deficiency anemia and heart failure with reduced left ventricular ejection fraction, and it may also lead to a decrease in cardiovascular events.
Effect of ferric derisomaltose on cardiovascular and non-cardiovascular events in patients with iron deficiency anemia and heart failure
Effect of ferric derisomaltose on cardiovascular and non-cardiovascular events in patients with iron deficiency anemia and heart failure
A recent study found that the administration of intravenous ferric derisomaltose (FDI) in patients diagnosed with both iron deficiency anemia and heart failure with reduced left ventricular ejection fraction has been found to improve their quality of life and may decrease cardiovascular events. This study’s results were published in the Journal of Cardiac Failure.
In the IRONMAN trial, patients with heart failure, iron deficiency (ferritin <100 µg/L or transferrin saturation of <20%), and a left ventricular ejection fraction of ≤45% were enrolled. Out of the total, 68% (n= 771) had anemia (hemoglobin less than 12 g/dL for women and less than 13 g/dL for men). Patients were then randomly assigned to either FDI (n = 397) or usual care (n = 374) and were followed for a median duration of 2.6 years. The primary endpoint of the study was recurrent hospitalization for heart failure and cardiovascular death.
The occurrence of recurrent hospitalization for heart failure and cardiovascular death was less frequent among individuals assigned to FDI (rate ratio 0.78, 95% confidence interval of 0.61-1.01, and the p-value = 0.063). Similarly, the first event analysis for cardiovascular hospitalization or death for heart failure showed similar results (hazard ratio of 0.77, 95% confidence interval of 0.62-0.96 ; p-value = 0.022). Additionally, patients who were randomized to FDI reported better quality of life scores for overall (p-value = 0.013) and physical domain (p-value = 0.00093) at 4 months, as measured by the Minnesota Living with Heart Failure questionnaire.
The above study demonstrated that the administration of intravenous FDI improves the quality of life in patients diagnosed with both iron deficiency anemia and heart failure with reduced left ventricular ejection fraction, and it may also lead to a decrease in cardiovascular events.
Comparison of an "inclisiran first" approach with standard care for patients diagnosed with atherosclerotic cardiovascular disease
Comparison of an "inclisiran first" approach with standard care for patients diagnosed with atherosclerotic cardiovascular disease
A recent study showed that the use of an "inclisiran first" approach resulted in a more significant reduction in low-density lipoprotein cholesterol (LDL-C) levels when compared to standard care, without negatively impacting the use of statins or giving rise to any additional safety concerns. This research findings were published in the Journal of the American College of Cardiology.
The VICTORION-INITIATE trial involved 450 patients who were randomly assigned in a 1:1 ratio to receive either inclisiran (284 mg at days 0, 90, and 270) along with standard care (lipid management determined by the treating physician) or standard care alone. The primary endpoints of the study assessed the percentage change in LDL-C levels from the baseline and the rates of statin discontinuation.
The "inclisiran first" strategy resulted in significantly larger reductions in LDL-C levels from baseline to day 330 compared to standard care (60.0% vs. 7.0%; P < 0.001). The discontinuation rates of statins with the "inclisiran first" approach (6.0%) were found to be noninferior to standard care (16.7%). A higher proportion of patients in the "inclisiran first" group achieved their LDL-C goals compared to standard care (<70 mg/dL: 81.8% vs. 22.2%; <55 mg/dL: 71.6% vs. 8.9%; P < 0.001). Rates of treatment-emergent adverse events (TEAE) and serious TEAE were comparable between the two treatment strategies (62.8% vs. 53.7% and 11.5% vs. 13.4%, respectively).
The above study demonstrated that adopting an "inclisiran first" strategy led to a greater decrease in LDL-C levels compared to conventional treatment, while maintaining the use of statins and without posing any additional safety issues.
Comparison of an "inclisiran first" approach with standard care for patients diagnosed with atherosclerotic cardiovascular disease
Comparison of an "inclisiran first" approach with standard care for patients diagnosed with atherosclerotic cardiovascular disease
A recent study showed that the use of an "inclisiran first" approach resulted in a more significant reduction in low-density lipoprotein cholesterol (LDL-C) levels when compared to standard care, without negatively impacting the use of statins or giving rise to any additional safety concerns. This research findings were published in the Journal of the American College of Cardiology.
The VICTORION-INITIATE trial involved 450 patients who were randomly assigned in a 1:1 ratio to receive either inclisiran (284 mg at days 0, 90, and 270) along with standard care (lipid management determined by the treating physician) or standard care alone. The primary endpoints of the study assessed the percentage change in LDL-C levels from the baseline and the rates of statin discontinuation.
The "inclisiran first" strategy resulted in significantly larger reductions in LDL-C levels from baseline to day 330 compared to standard care (60.0% vs. 7.0%; P < 0.001). The discontinuation rates of statins with the "inclisiran first" approach (6.0%) were found to be noninferior to standard care (16.7%). A higher proportion of patients in the "inclisiran first" group achieved their LDL-C goals compared to standard care (<70 mg/dL: 81.8% vs. 22.2%; <55 mg/dL: 71.6% vs. 8.9%; P < 0.001). Rates of treatment-emergent adverse events (TEAE) and serious TEAE were comparable between the two treatment strategies (62.8% vs. 53.7% and 11.5% vs. 13.4%, respectively).
The above study demonstrated that adopting an "inclisiran first" strategy led to a greater decrease in LDL-C levels compared to conventional treatment, while maintaining the use of statins and without posing any additional safety issues.
Nomogram predicts cancer-specific survival for patients with primary gastrointestinal melanoma
Nomogram predicts cancer-specific survival for patients with primary gastrointestinal melanoma
According to a recent study, it was validated that nomogram can predict cancer-specific survival and develop a risk stratification system for patients with primary gastrointestinal melanoma. The findings of the study were published in The Turkish Journal of Gastroenterology.
Results from a database of 433 patients with primary gastrointestinal melanoma were included in the study after randomly dividing the participants into training and validation cohorts (8:2). The nomogram was constructed based on the risk factors identified in the multivariate Cox regression analysis. Based on the nomogram, a risk stratification system was developed. Time-dependent receiver operating characteristic, calibration curve, and decision curve analysis were performed.
All cases were randomly divided into either the training (n = 347, 80%) or validation cohort (n = 86, 20%). For all patients, the median cancer-specific survival (CSS) time was 18.0 months (95% CI: 14.7-21.3). The median CSS was 18.0 months (95% CI: 14.5-21.5) and 18.0 months (95% CI: 10.7-25.3) in the training and validation cohorts, respectively (log-rank test, P = .241).
It was found that CSS under the curves of the nomogram for 6-, 12-, and 18-month were 0.789, 0.757, and 0.726 for internal validation, and 0.796, 0.763, and 0.795 for the external validation. Furthermore, the patients were divided into 2 risk sub-groups to study the risk stratification, low-risk (point: 0-182) and high-risk (point: 183-333). The median CSS was 31.0 months (95% CI: 24.5-37.5) in the low-risk subgroup and 8.0 months (95% CI: 6.2-9.8) in the high-risk subgroup. The Kaplan-Meier analysis and the log-rank test demonstrated that the risk stratification was well-differentiated in patients with varying risks of cancer-specific survival.
Thus, it can be concluded that the nomogram prediction model may be practical for validation of cancer-specific survival and development of a risk stratification system in patients with primary gastrointestinal melanoma.
Nomogram predicts cancer-specific survival for patients with primary gastrointestinal melanoma
Nomogram predicts cancer-specific survival for patients with primary gastrointestinal melanoma
According to a recent study, it was validated that nomogram can predict cancer-specific survival and develop a risk stratification system for patients with primary gastrointestinal melanoma. The findings of the study were published in The Turkish Journal of Gastroenterology.
Results from a database of 433 patients with primary gastrointestinal melanoma were included in the study after randomly dividing the participants into training and validation cohorts (8:2). The nomogram was constructed based on the risk factors identified in the multivariate Cox regression analysis. Based on the nomogram, a risk stratification system was developed. Time-dependent receiver operating characteristic, calibration curve, and decision curve analysis were performed.
All cases were randomly divided into either the training (n = 347, 80%) or validation cohort (n = 86, 20%). For all patients, the median cancer-specific survival (CSS) time was 18.0 months (95% CI: 14.7-21.3). The median CSS was 18.0 months (95% CI: 14.5-21.5) and 18.0 months (95% CI: 10.7-25.3) in the training and validation cohorts, respectively (log-rank test, P = .241).
It was found that CSS under the curves of the nomogram for 6-, 12-, and 18-month were 0.789, 0.757, and 0.726 for internal validation, and 0.796, 0.763, and 0.795 for the external validation. Furthermore, the patients were divided into 2 risk sub-groups to study the risk stratification, low-risk (point: 0-182) and high-risk (point: 183-333). The median CSS was 31.0 months (95% CI: 24.5-37.5) in the low-risk subgroup and 8.0 months (95% CI: 6.2-9.8) in the high-risk subgroup. The Kaplan-Meier analysis and the log-rank test demonstrated that the risk stratification was well-differentiated in patients with varying risks of cancer-specific survival.
Thus, it can be concluded that the nomogram prediction model may be practical for validation of cancer-specific survival and development of a risk stratification system in patients with primary gastrointestinal melanoma.
Inorganic nitrate reduces contrast-induced nephropathy following coronary angiography for acute coronary syndromes
Inorganic nitrate reduces contrast-induced nephropathy following coronary angiography for acute coronary syndromes
A recent study demonstrated that for patients at risk of renal injury undergoing coronary angiography for acute coronary syndromes (ACS), a short (5-day) regimen of once-daily inorganic nitrate resulted in decreased contrast-induced nephropathy (CIN), enhanced kidney outcomes at 3 months, and reduced major adverse cardiovascular events (MACE) at 1 year when compared with individuals who received a placebo. This study’s results were published in the European Heart Journal.
The NITRATE-CIN trial was a double-blind, randomized, placebo-controlled trial that included a total of 640 patients. These patients were randomized to receive either once daily potassium nitrate (n= 319; 12 mmol) or placebo (n= 321; potassium chloride) capsules for a period of 5 days. The primary endpoint of the trial was the incidence of CIN based on KDIGO criteria. Secondary outcomes measured included kidney function (eGFR) at 3 months, rates of procedural myocardial infarction, and MACE at 12 months.
Inorganic nitrate treatment led to a significant decrease in the rates of CIN compared to the placebo (9.1% vs 30.5%). This difference remained even after adjusting for baseline creatinine levels and diabetes status. Additionally, the use of inorganic nitrate exhibited positive outcomes in secondary outcomes, including a lower incidence of procedural myocardial infarction (2.7% vs 12.5%), improved renal function at 3 months (between-group change in estimated glomerular filtration rate of 5.17), and a reduced occurrence of MACE at 1 year (9.1% vs. 18.1%) compared to the placebo group.
Thus, it can be concluded that a 5-day regimen of once-daily inorganic nitrate may be beneficial for patients undergoing coronary angiography for ACS. This treatment resulted in a decrease in CIN, improved kidney outcomes at 3 months, and reduced MACE at 1 year compared to those who received a placebo.
Inorganic nitrate reduces contrast-induced nephropathy following coronary angiography for acute coronary syndromes
Inorganic nitrate reduces contrast-induced nephropathy following coronary angiography for acute coronary syndromes
A recent study demonstrated that for patients at risk of renal injury undergoing coronary angiography for acute coronary syndromes (ACS), a short (5-day) regimen of once-daily inorganic nitrate resulted in decreased contrast-induced nephropathy (CIN), enhanced kidney outcomes at 3 months, and reduced major adverse cardiovascular events (MACE) at 1 year when compared with individuals who received a placebo. This study’s results were published in the European Heart Journal.
The NITRATE-CIN trial was a double-blind, randomized, placebo-controlled trial that included a total of 640 patients. These patients were randomized to receive either once daily potassium nitrate (n= 319; 12 mmol) or placebo (n= 321; potassium chloride) capsules for a period of 5 days. The primary endpoint of the trial was the incidence of CIN based on KDIGO criteria. Secondary outcomes measured included kidney function (eGFR) at 3 months, rates of procedural myocardial infarction, and MACE at 12 months.
Inorganic nitrate treatment led to a significant decrease in the rates of CIN compared to the placebo (9.1% vs 30.5%). This difference remained even after adjusting for baseline creatinine levels and diabetes status. Additionally, the use of inorganic nitrate exhibited positive outcomes in secondary outcomes, including a lower incidence of procedural myocardial infarction (2.7% vs 12.5%), improved renal function at 3 months (between-group change in estimated glomerular filtration rate of 5.17), and a reduced occurrence of MACE at 1 year (9.1% vs. 18.1%) compared to the placebo group.
Thus, it can be concluded that a 5-day regimen of once-daily inorganic nitrate may be beneficial for patients undergoing coronary angiography for ACS. This treatment resulted in a decrease in CIN, improved kidney outcomes at 3 months, and reduced MACE at 1 year compared to those who received a placebo.
How would you rate this Medshorts
Thank you !
Your rating has been recorded.
Videos Speakers
Want our representative to contact you ?
Below fields are needed for webinar purpose.





































