Why Daplo
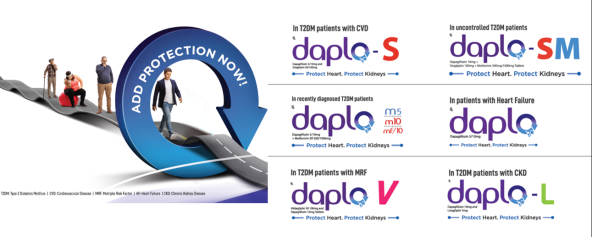
Daplo (Dr.Reddy’s brand of dapagliflozin) is 100% Bio-equivalent to Innovator. There is NO Bio-variability with Daplo, More than 70% of the drug is released from a tablet in 20 min. Daplo has superior packaging which ensures greater protection. PROTECT HEART. PROTECT KIDNEYS of every Diabetes patient with Daplo & Daplo M.
About Dapagliflozin
It helps get rid of excess glucose from the body through urine. Lowering blood glucose levels is an essential part of managing diabetes. It can also be taken together with other diabetes medicines when a single medicine is not controlling your blood sugar properly.
Dapagliflozin reduces the risk of hospitalization for heart failure in adults with type 2 diabetes mellitus and either established cardiovascular (CV) disease or multiple CV risk factors.
Dapagliflozin reduces the risk of sustained eGFR decline, end‑stage kidney disease, cardiovascular death, and hospitalization for heart failure in adults with chronic kidney disease at risk of progression.
Dapagliflozin reduces the risk of cardiovascular death and hospitalization for heart failure in adults with heart failure (NYHA class II-IV) with reduced ejection fraction.
Where to use?
In Type 2 diabetes mellitus
Expert's View
Monthly Newsletters
Trial Outcomes
Frequently Asked Questions
No, Sodium-Glucose Co-transporter 2 (SGLT2) inhibitors induced natriuresis is transient. There are compensatory mechanisms that increases the re-absorption of NA+ ions at other nephron sites. A new steady state is established by terminating negative NA+ ions and maintaining the balance eventually. (https://diabetes.diabetesjournals.org/content/68/6/1109).
Treatment with SGLT2 inhibitors leads to dehydration if the water intake is not sufficient. The patient should remain adequately hydrated (not more than normal). SGLT2 inhibitors should be withheld in patients with poor nutritional or hydration status. (https://www.uspharmacist.com/article/benefits-and-complications-of-sodiumglucose-cotransporter-2-inhibitors) (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5812257/).
Though weight loss is an effect of SGLT2 inhibitors, it is not indicated to use in any weight loss or weight management process. However, when used for the approved indications like T2DM, SGLT2 inhibitors do produce weight loss.
No, Diuretics may have only diuretic activity. Apart from their diuretic activity, SGLT2 inhibitors protect the kidney by reducing the rate at which eGFR declines in patients with diabetic nephropathy. In addition to their diuretic activity, DAPA also improves Glycemic control and long-term CV or renal outcomes.
Unlike other SGLT2 inhibitors, DAPA is supported with data in T2DM patients (DECLARE TIMI) with multiple risk factors (primary prevention population). So, it is the ideal choice in the case of T2DM patients with multiple CV risk factors. DAPA is also well studied for use and fit for use in HF patients with reduced ejection fraction (HFrEF). It can also be used in non-diabetic patients for CV & renal (DAPA CKD) protection.
Yes, it can be prescribed to kidney-impaired patients. Whether the patient is suitable for SGLT2 inhibitors, is decided based on the renal function (eGFR)/stage of CKD. DAPA should not be initiated in patients with a GFR < 60 mL/min. In case the patient is already on DAPA, it should be discontinued, if GFR is persistently below 45 mL/min. DAPA is contraindicated if eGFR is less than 30 mL/min.
Yes, DAPA can be given in early diabetes. It can be used for initial monotherapy or initial combination therapy. DAPA, especially in those with ASCVD/HF/CKD, will have better CV & renal outcomes when initiated early.
Increased incidence of UTI is a known side effect of SGLT2 inhibitors. However, not everyone will develop UTIs. The incidence of UTIs with DAPA varies from 1.5% in DECLARE TIMI (incidence of UTIs with Placebo was 1.6%) to 5.7% in pooled studies. Meta-analysis of trials and a large population-based cohort study have shown no increased risk, which provides important reassurance for patients and prescribers. (https://www.nature.com/articles/s41574-019-0275-6). Meta-analysis of randomized controlled trials (RCTs) showed no significant difference in UTIs between SGLT2 inhibitors versus Control. (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5460243/).
DAPA should not be initiated in patients with a GFR < 60mL/min. In case the patient is already on DAPA, it should be discontinued if the GFR is persistently below 45 mL/min. DAPA is contraindicated if eGFR is less than 30 mL/min.
The incidence of UTIs with DAPA varies from 1.5% in DECLARE TIMI (incidence of UTIs with placebo was 1.6%) to 5.7% in pooled studies.
Unlike other SGLT2 inhibitors, DAPA is supported with research studies in T2DM patients (DECLARE TIMI) with multiple risk factors (primary prevention population). So, it is the ideal choice in the case of T2DM patients with multiple CV risk factors. DAPA is supported with studies and fit for use in HF patients with reduced ejection fraction (HFrEF). DAPA is supported with studies and fit for use even in non-diabetic patients for CV & renal (DAPA CKD) protection that it offers.
Yes, for Glycemic control in T2DM patients with CKD, 5mg can be given. In case, DAPA is being prescribed for benefits beyond Glycemic control (CV & renal protection), which is the practice, 10mg must be given (DAPA CKD trial).
The incidence of Diabetic Ketoacidosis with DAPA in DECLARE TIMI, was 0.3%. In this case, initiating DAPA is recommended to prevent flaring up of the infection.
DAPA is not approved for use in dialysis patients.
No, dose modification is needed in mild, moderate, and severe hepatic impairment. However, in severe cases, it should be individually assessed as there are no studies in such a population.
Though weight loss is an effect of SGLT2 inhibitors, it is not indicated to use in any weight loss or weight management process. However, when used for the approved indications like T2DM, SGLT2Is does result in weight loss.
DAPA is not a substitute for anti-hypertensive agents. The decision to modify the ARBs/anti-hypertensive dose should be taken on a case-to-case basis, based on the individual BP goals.
A T2DM patient is already at a higher risk of UTI. Though the risk of UTI is increased by SGLT2Is, UTIs can be managed in most cases through early detection and appropriate treatment (along with health & hygiene), which may cost less than treating long-term CV & renal complications of T2DM. At the same time, SGLT2Is offer several benefits beyond Glycemic control, which in the long run improve the QOL. Dapagliflozin showed a more favorable benefit on Japanese T2DM patients’ QOL vs DPP4is (https://link.springer.com/article/10.1007/s13300-020-00941-8). Dapagliflozin improved symptoms, physical function, and quality of life in patients with heart failure and reduced ejection fraction (https://pubmed.ncbi.nlm.nih.gov/31736335/).
SGLT2 inhibitors have a low risk of Hypoglycemia, weight loss, decrease in BP & other benefits beyond Glycemic control (CV & renal protection).
Sodium-glucose Cotransporter2 (SGLT2) inhibitors are recommended in ASCVD/CKD/HF patients as first add on.
9 hours is considered as half-life of DAPA.
Yes, it can be taken with or without food.
DAPA is approved only in T2DM and heart failure.
The dosage is 5mg or 10mg OD.
The dosage for beyond Glycemic control is 10 mg OD.
In case of heart failure, the DAPA dosage is 10mg OD.
DAPA is contraindicated in case DAPA is less than 30 mL/min.
Yes, it can be used in treatment naïve T2DM patients as initial monotherapy or initial combination therapy.
The drug classes include: Metformin, SUs, TZDs, DPP4Is, GLP1RAs & Insulin.
Yes, DAPA decreases the insulin dose requirement
The CVOT is DECLARE TIMI.
The study is DAPA HF.
The study is DAPA CKD.
The SGLT2I is DAPA (DECLARE TIMI).
Yes, DECLRE TIMI can be used in this case.
Yes, DAPA HFrEF can be used in this case.
Yes, the risk of hospitalization due to heart failure is reduced.
Yes, DAPA reduces the risk of kidney failure.



















