test
test
test
test
test
test
test
test
test
test
Webinars
Videos
Managing Weight with Celevida
Celevida contains High Fibre and provides upto 3 hours satiety. It keeps you full and helps in managing weight.
Managing Weight with Celevida
Celevida contains High Fibre and provides upto 3 hours satiety. It keeps you full and helps in managing weight.
Managing Weight with Celevida
Celevida contains High Fibre and provides upto 3 hours satiety. It keeps you full and helps in managing weight.
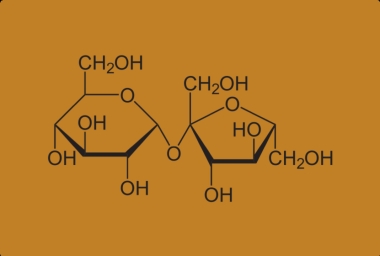
What Makes Celevida Sweet?
Celevida contains Sucralose. It has no added sugar and safe to consume for Diabetics aswell
What Makes Celevida Sweet?
Celevida contains Sucralose. It has no added sugar and safe to consume for Diabetics aswell
What Makes Celevida Sweet?
Celevida contains Sucralose. It has no added sugar and safe to consume for Diabetics aswell
Courses
Medshorts

Superior weight reduction with tirzepatide independent of gastrointestinal adverse events in people with type 2 diabetes
A recent study suggests that people with type 2 diabetes showed superior weight reduction with tirzepatide, independent of gastrointestinal (GI) adverse events (AEs) and nausea, vomiting or diarrhoea (N/V/D). This study was published in the journal, Diabetes, Obesity & Metabolism.
The post hoc analysis of the SURPASS -1 to -5 clinical trials included 6263 participants whose treatment for type 2 diabetes involved a random assignment to receive tirzepatide (5, 10, or 15 mg) once a week as monotherapy or in addition to baseline antihyperglycemic medication(s) as a comparator (placebo, semaglutide 1 mg once a week, or titrated daily basal insulins). The participants self-reported (yes/no) for any N/V/D or GI AEs. Change in body weight was assessed from baseline within each trial and subgroup. Mediation analyses to study the effects of tirzepatide on weight change were conducted.
At the end of the study period, nausea (12%-24%), vomiting (2%-13%), and diarrhoea (12%-22%) were the most commonly reported GI AEs with tirzepatide. The mean weight reduction was significantly greater with tirzepatide when compared to the placebo, with consistency being maintained between participants who reported N/V/D and those who didn’t. At the primary timepoint, individuals who experienced N/V/D symptoms showed weight reduction ranging from -6.2 to -14.9 kg, while those without these symptoms had a mean weight reduction ranging from -6.2 to -13.3 kg. According to the median analyses, there was only a minimal contribution with N/V/D and GI AEs to the overall difference in weight change.
From the above results, it can be concluded that superior weight reduction observed with tirzepatide when compared to other comparators appears to be independent of N/V/D or GI AEs.

Superior weight reduction with tirzepatide independent of gastrointestinal adverse events in people with type 2 diabetes
A recent study suggests that people with type 2 diabetes showed superior weight reduction with tirzepatide, independent of gastrointestinal (GI) adverse events (AEs) and nausea, vomiting or diarrhoea (N/V/D). This study was published in the journal, Diabetes, Obesity & Metabolism.
The post hoc analysis of the SURPASS -1 to -5 clinical trials included 6263 participants whose treatment for type 2 diabetes involved a random assignment to receive tirzepatide (5, 10, or 15 mg) once a week as monotherapy or in addition to baseline antihyperglycemic medication(s) as a comparator (placebo, semaglutide 1 mg once a week, or titrated daily basal insulins). The participants self-reported (yes/no) for any N/V/D or GI AEs. Change in body weight was assessed from baseline within each trial and subgroup. Mediation analyses to study the effects of tirzepatide on weight change were conducted.
At the end of the study period, nausea (12%-24%), vomiting (2%-13%), and diarrhoea (12%-22%) were the most commonly reported GI AEs with tirzepatide. The mean weight reduction was significantly greater with tirzepatide when compared to the placebo, with consistency being maintained between participants who reported N/V/D and those who didn’t. At the primary timepoint, individuals who experienced N/V/D symptoms showed weight reduction ranging from -6.2 to -14.9 kg, while those without these symptoms had a mean weight reduction ranging from -6.2 to -13.3 kg. According to the median analyses, there was only a minimal contribution with N/V/D and GI AEs to the overall difference in weight change.
From the above results, it can be concluded that superior weight reduction observed with tirzepatide when compared to other comparators appears to be independent of N/V/D or GI AEs.


Superior weight reduction with tirzepatide independent of gastrointestinal adverse events in people with type 2 diabetes
A recent study suggests that people with type 2 diabetes showed superior weight reduction with tirzepatide, independent of gastrointestinal (GI) adverse events (AEs) and nausea, vomiting or diarrhoea (N/V/D). This study was published in the journal, Diabetes, Obesity & Metabolism.
The post hoc analysis of the SURPASS -1 to -5 clinical trials included 6263 participants whose treatment for type 2 diabetes involved a random assignment to receive tirzepatide (5, 10, or 15 mg) once a week as monotherapy or in addition to baseline antihyperglycemic medication(s) as a comparator (placebo, semaglutide 1 mg once a week, or titrated daily basal insulins). The participants self-reported (yes/no) for any N/V/D or GI AEs. Change in body weight was assessed from baseline within each trial and subgroup. Mediation analyses to study the effects of tirzepatide on weight change were conducted.
At the end of the study period, nausea (12%-24%), vomiting (2%-13%), and diarrhoea (12%-22%) were the most commonly reported GI AEs with tirzepatide. The mean weight reduction was significantly greater with tirzepatide when compared to the placebo, with consistency being maintained between participants who reported N/V/D and those who didn’t. At the primary timepoint, individuals who experienced N/V/D symptoms showed weight reduction ranging from -6.2 to -14.9 kg, while those without these symptoms had a mean weight reduction ranging from -6.2 to -13.3 kg. According to the median analyses, there was only a minimal contribution with N/V/D and GI AEs to the overall difference in weight change.
From the above results, it can be concluded that superior weight reduction observed with tirzepatide when compared to other comparators appears to be independent of N/V/D or GI AEs.

Effects of ipragliflozin and sitagliptin on serum lipid and apolipoprotein profiles in type 2 diabetes
According to a recent study, ipragliflozin may have an anti-atherogenic effect through modulation of apoE(Apolipoprotein E) and HDL-C(High-density lipoprotein cholesterol) when compared to sitagliptinthrough apo B48 (Apolipoprotein B48) and TG(Triglycerides),CII, and CIII in type 2 diabetic patients. The results of this study were published in the journal, Cardiovascular Diabetology.
The SUCRE study was a multicenter, open-label, randomized, controlled trial that included 20-74 years old patients with type 2 diabetes. These patients had serum triglyceride levels of 120-399 mg/dL and HbA1c levels of 7.0-10.5% and/or were on oral hypoglycemic agents. These subjects were randomized to receive either 50 mg/day of ipragliflozin (n=77) or 50 mg/day of sitagliptin (n=83). The clinical parameters were measured at 0, 1, 3, and 6 months following the treatment.
At the end of the study, both ipragliflozin and sitagliptin showed reduced levels of fasting plasma glucose, HbA1c, and glycoalbumin. While ipragliflozin increased HDL-C while decreasing apo E, sitagliptin increased LDL-C (Low-density lipoprotein cholesterol) while decreasing TG, CII, CIII, and apo B48. For HDL-C and apo B48, the differences between treatments were significant but for apo A1, they were almost significant. Additionally, ipragliflozin reduced blood pressure, body weight, uric acid, serum liver enzymes, and leptin and increased serum ketones.
Based on the above results, it can be concluded that although ipragliflozin and sitagliptin may affect glycemic parameters in a similar manner, their effects on serum lipid and apolipoprotein profiles may be different. Therefore, ipragliflozin may have an anti-atherogenic effect in patients with type 2 diabetes compared to sitagliptin through modulation of HDL-C and apo E.

Effects of ipragliflozin and sitagliptin on serum lipid and apolipoprotein profiles in type 2 diabetes
According to a recent study, ipragliflozin may have an anti-atherogenic effect through modulation of apoE(Apolipoprotein E) and HDL-C(High-density lipoprotein cholesterol) when compared to sitagliptinthrough apo B48 (Apolipoprotein B48) and TG(Triglycerides),CII, and CIII in type 2 diabetic patients. The results of this study were published in the journal, Cardiovascular Diabetology.
The SUCRE study was a multicenter, open-label, randomized, controlled trial that included 20-74 years old patients with type 2 diabetes. These patients had serum triglyceride levels of 120-399 mg/dL and HbA1c levels of 7.0-10.5% and/or were on oral hypoglycemic agents. These subjects were randomized to receive either 50 mg/day of ipragliflozin (n=77) or 50 mg/day of sitagliptin (n=83). The clinical parameters were measured at 0, 1, 3, and 6 months following the treatment.
At the end of the study, both ipragliflozin and sitagliptin showed reduced levels of fasting plasma glucose, HbA1c, and glycoalbumin. While ipragliflozin increased HDL-C while decreasing apo E, sitagliptin increased LDL-C (Low-density lipoprotein cholesterol) while decreasing TG, CII, CIII, and apo B48. For HDL-C and apo B48, the differences between treatments were significant but for apo A1, they were almost significant. Additionally, ipragliflozin reduced blood pressure, body weight, uric acid, serum liver enzymes, and leptin and increased serum ketones.
Based on the above results, it can be concluded that although ipragliflozin and sitagliptin may affect glycemic parameters in a similar manner, their effects on serum lipid and apolipoprotein profiles may be different. Therefore, ipragliflozin may have an anti-atherogenic effect in patients with type 2 diabetes compared to sitagliptin through modulation of HDL-C and apo E.


Effects of ipragliflozin and sitagliptin on serum lipid and apolipoprotein profiles in type 2 diabetes
According to a recent study, ipragliflozin may have an anti-atherogenic effect through modulation of apoE(Apolipoprotein E) and HDL-C(High-density lipoprotein cholesterol) when compared to sitagliptinthrough apo B48 (Apolipoprotein B48) and TG(Triglycerides),CII, and CIII in type 2 diabetic patients. The results of this study were published in the journal, Cardiovascular Diabetology.
The SUCRE study was a multicenter, open-label, randomized, controlled trial that included 20-74 years old patients with type 2 diabetes. These patients had serum triglyceride levels of 120-399 mg/dL and HbA1c levels of 7.0-10.5% and/or were on oral hypoglycemic agents. These subjects were randomized to receive either 50 mg/day of ipragliflozin (n=77) or 50 mg/day of sitagliptin (n=83). The clinical parameters were measured at 0, 1, 3, and 6 months following the treatment.
At the end of the study, both ipragliflozin and sitagliptin showed reduced levels of fasting plasma glucose, HbA1c, and glycoalbumin. While ipragliflozin increased HDL-C while decreasing apo E, sitagliptin increased LDL-C (Low-density lipoprotein cholesterol) while decreasing TG, CII, CIII, and apo B48. For HDL-C and apo B48, the differences between treatments were significant but for apo A1, they were almost significant. Additionally, ipragliflozin reduced blood pressure, body weight, uric acid, serum liver enzymes, and leptin and increased serum ketones.
Based on the above results, it can be concluded that although ipragliflozin and sitagliptin may affect glycemic parameters in a similar manner, their effects on serum lipid and apolipoprotein profiles may be different. Therefore, ipragliflozin may have an anti-atherogenic effect in patients with type 2 diabetes compared to sitagliptin through modulation of HDL-C and apo E.

Efficacy and safety of bempedoic acid in patients with and without diabetes
A recent study demonstrated that bempedoic acid reduces LDL cholesterol and high-sensitivity C-reactive protein and the risk of cardiovascular events in both Diabetic and non-diabetic patients .The findings of this study were published in the journal, Lancet. Diabetes & Endocrinology.
CLEAR Outcomes was a randomised, double-blind, placebo-controlled trial that included 13,970 patients, who were randomly assigned to those with diabetes (n=6373), prediabetes (n= 5796), and normoglycaemia (n=1801). Patients with or without cardiovascular disease who were unwilling or unable to adhere to the recommended doses of statins and an LDL cholesterol of 2·59 mmol/L or more were randomly assigned (1:1) to receive either bempedoic acid 180 mg once per day or placebo. Using the intention-to-treat population stratified by baseline glycaemia status, the efficacy endpoint of the prespecified analysis was a time-to-event analysis of four-component major adverse cardiovascular event (MACE-4), which is the composite of nonfatal myocardial infarction, cardiovascular death, nonfatal stroke, or coronary revascularisation. At baseline, the risk of new-onset diabetes and HbA1c increase was analysed in patients without diabetes.
After a median follow-up of 3.4 years, patients with diabetes had significant relative and absolute cardiovascular risk reductions in MACE-4 endpoints with bempedoic acid (absolute risk reduction of 2·4%) compared to the placebo. The incidence of new-onset diabetes was comparable in both the bempedoic acid and placebo groups. The HbA1c concentrations were similar between randomised groups in patients who had prediabetes and normoglycaemia, at 12 months and end of the study. Placebo-corrected LDL cholesterol concentrations and high-sensitivity C-reactive protein at 6 months showed reductions in each glycaemic stratum (diabetes, prediabetes, and normoglycemia) for patients who were randomly assigned to bempedoic acid.
It was observed that bempedoic acid reduces LDL cholesterol and high-sensitivity C-reactive protein and the risk of cardiovascular events among patients with diabetes. With bempedoic acid, participants without diabetes had no increase in new-onset diabetes or worsening HbA1c. Based on the findings of this study, it can be concluded that the efficacy and cardiometabolic safety profile of bempedoic acid makes it a valuable clinical option for those with and without diabetes.

Efficacy and safety of bempedoic acid in patients with and without diabetes
A recent study demonstrated that bempedoic acid reduces LDL cholesterol and high-sensitivity C-reactive protein and the risk of cardiovascular events in both Diabetic and non-diabetic patients .The findings of this study were published in the journal, Lancet. Diabetes & Endocrinology.
CLEAR Outcomes was a randomised, double-blind, placebo-controlled trial that included 13,970 patients, who were randomly assigned to those with diabetes (n=6373), prediabetes (n= 5796), and normoglycaemia (n=1801). Patients with or without cardiovascular disease who were unwilling or unable to adhere to the recommended doses of statins and an LDL cholesterol of 2·59 mmol/L or more were randomly assigned (1:1) to receive either bempedoic acid 180 mg once per day or placebo. Using the intention-to-treat population stratified by baseline glycaemia status, the efficacy endpoint of the prespecified analysis was a time-to-event analysis of four-component major adverse cardiovascular event (MACE-4), which is the composite of nonfatal myocardial infarction, cardiovascular death, nonfatal stroke, or coronary revascularisation. At baseline, the risk of new-onset diabetes and HbA1c increase was analysed in patients without diabetes.
After a median follow-up of 3.4 years, patients with diabetes had significant relative and absolute cardiovascular risk reductions in MACE-4 endpoints with bempedoic acid (absolute risk reduction of 2·4%) compared to the placebo. The incidence of new-onset diabetes was comparable in both the bempedoic acid and placebo groups. The HbA1c concentrations were similar between randomised groups in patients who had prediabetes and normoglycaemia, at 12 months and end of the study. Placebo-corrected LDL cholesterol concentrations and high-sensitivity C-reactive protein at 6 months showed reductions in each glycaemic stratum (diabetes, prediabetes, and normoglycemia) for patients who were randomly assigned to bempedoic acid.
It was observed that bempedoic acid reduces LDL cholesterol and high-sensitivity C-reactive protein and the risk of cardiovascular events among patients with diabetes. With bempedoic acid, participants without diabetes had no increase in new-onset diabetes or worsening HbA1c. Based on the findings of this study, it can be concluded that the efficacy and cardiometabolic safety profile of bempedoic acid makes it a valuable clinical option for those with and without diabetes.


Efficacy and safety of bempedoic acid in patients with and without diabetes
A recent study demonstrated that bempedoic acid reduces LDL cholesterol and high-sensitivity C-reactive protein and the risk of cardiovascular events in both Diabetic and non-diabetic patients .The findings of this study were published in the journal, Lancet. Diabetes & Endocrinology.
CLEAR Outcomes was a randomised, double-blind, placebo-controlled trial that included 13,970 patients, who were randomly assigned to those with diabetes (n=6373), prediabetes (n= 5796), and normoglycaemia (n=1801). Patients with or without cardiovascular disease who were unwilling or unable to adhere to the recommended doses of statins and an LDL cholesterol of 2·59 mmol/L or more were randomly assigned (1:1) to receive either bempedoic acid 180 mg once per day or placebo. Using the intention-to-treat population stratified by baseline glycaemia status, the efficacy endpoint of the prespecified analysis was a time-to-event analysis of four-component major adverse cardiovascular event (MACE-4), which is the composite of nonfatal myocardial infarction, cardiovascular death, nonfatal stroke, or coronary revascularisation. At baseline, the risk of new-onset diabetes and HbA1c increase was analysed in patients without diabetes.
After a median follow-up of 3.4 years, patients with diabetes had significant relative and absolute cardiovascular risk reductions in MACE-4 endpoints with bempedoic acid (absolute risk reduction of 2·4%) compared to the placebo. The incidence of new-onset diabetes was comparable in both the bempedoic acid and placebo groups. The HbA1c concentrations were similar between randomised groups in patients who had prediabetes and normoglycaemia, at 12 months and end of the study. Placebo-corrected LDL cholesterol concentrations and high-sensitivity C-reactive protein at 6 months showed reductions in each glycaemic stratum (diabetes, prediabetes, and normoglycemia) for patients who were randomly assigned to bempedoic acid.
It was observed that bempedoic acid reduces LDL cholesterol and high-sensitivity C-reactive protein and the risk of cardiovascular events among patients with diabetes. With bempedoic acid, participants without diabetes had no increase in new-onset diabetes or worsening HbA1c. Based on the findings of this study, it can be concluded that the efficacy and cardiometabolic safety profile of bempedoic acid makes it a valuable clinical option for those with and without diabetes.